Navigating A Clinical Values Divide: Fostering Therapist Collaboration and Patient-Centered Care
I'd like to initiate a conversation on a topic within our field that often sparks intense debate. Many clinicians are deeply passionate about this subject, and my aim is to encourage an open and constructive dialogue.
The issue in question revolves around the ongoing shift in our professions from a primarily biomedical approach to a more holistic biopsychosocial (BPS) framework. This transformation has given rise to distinct identity groups within our professions, resulting in misunderstandings and disagreements.
You might have encountered these debates on social media, where individuals who strongly favour a biomedical perspective often criticise the BPS approach, sometimes even resorting to derogatory terms like "talk therapy." In contrast, supporters of a BPS model voice concerns about excessive service provision, treatment dependency issues, and costs. They occasionally label those from the biomedical camp as "outdated," "greedy," or "ignorant" of research.
It is important to acknowledge that both sides share a genuine commitment to prioritising the well-being of our patients. The different strategies they adopt reflect variations in the importance assigned to specific values. The name-calling likely stems from frustration that the other side may not fully appreciate the value in their own viewpoints.
Beneath all these disagreements lies the clinical challenge of determining the optimal duration and endpoint for a patient's treatment plan (the choice of intervention is also a keenly fought debate, but that is a separate discussion for another day). When it comes to treatment duration and frequency, some clinicians advocate for early discharge with a bias toward self-management, while others favour a more engaged, prolonged approach. Interestingly, both groups often point fingers at each other and argue, "You're wrong!"
In my view, neither side can claim to be definitively "correct." I would even take it a step further and argue that if a treatment plan is primarily influenced by our individual clinical values, potentially to the detriment of others, it becomes more of a therapist-centered approach rather than a patient-centered one. In this sense, both sides could be seen as lacking. As our team at Coogee Bay Physio grows, it's possible that we'll have team members with differing values and views on this topic. Rather than operating in an environment with simmering tensions over practice differences, I'd prefer to proactively address this potential issue by outlining a strategy that can help us work harmoniously while remaining true to our individual values.
CLinician to clinician harmony
How can we work toward this goal? It starts with the notion that genuinely patient-centred treatment planning requires clinicians to take a step back and contemplate the scope of their clinical values. It doesn't imply completely discarding these values, but rather, not letting them rigidly determine the treatment path. Instead, we can create room for our treatment plans to be influenced by the clinical values held by clinicians we might typically go to great lengths to differentiate ourselves from.
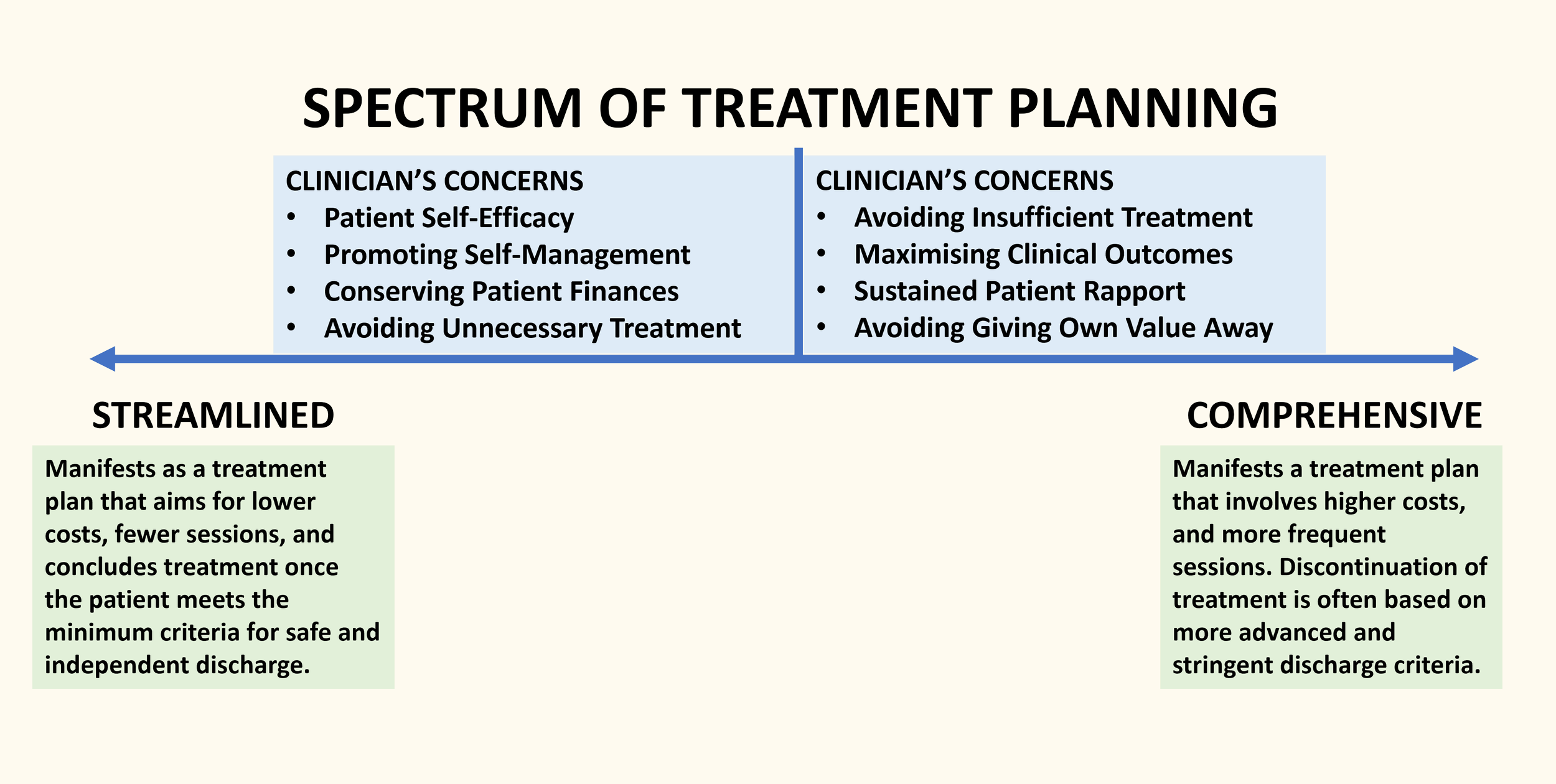
In this context, we can position both our own and others' clinical values along a spectrum. This spectrum serves as a guide for understanding treatment planning behaviours, including decisions about session frequency, duration, and discharge criteria. On one extreme of this spectrum, we find a streamlined, minimalist approach that places emphasis on preserving self-efficacy, minimising dependency, and managing costs efficiently. On the opposite end, we present a comprehensive approach that prioritises sustained and extended engagement between patients and therapists to achieve optimal clinical outcomes.
This spectrum allows us to better appreciate the merits of clinicians' approaches that we might otherwise struggle to see value in. It can help us from jumping to negative assumptions when we observe fellow clinicians planning and executing treatments in ways different from our own. In doing so, it can contribute to fostering a harmonious work environment by discouraging any overt criticism of divergent values or practices. Maintaining consistency of messaging for patients is important, especially when they are interacting with multiple team members. Receiving conflicting messages from different clinicians can hinder progress and lead to confusion for the patient.
patient centred treatment planning
Beyond fostering workplace harmony, acknowledging the diverse range of values guiding treatment planning significantly benefits patients. The most patient-centred approach, in my view, entails presenting plan options from both ends of the spectrum, enabling patients to choose their treatment path based on their values. Some may opt for streamlined treatment, while others may prefer a more comprehensive plan. The decision is the patients to make. Our job is to outline their options and ensure we have the skills and knowledge to support their preferred direction.
Putting this into practice can be challenging, particularly when a patient's preferred treatment path clashes with our own clinical values. For instance, a clinician who places a strong emphasis on education, reassurance, and early discharge to self-management as the ideal approach may find it difficult to formulate and deliver a more comprehensive plan comprising more elaborate interventions across more treatment sessions. On the other hand, a clinician with a stronger biomedical orientation might struggle with allowing a patient to opt for a "wait and see" approach, involving minimal intervention and potentially relying on natural symptom resolution. They might feel that they're not providing sufficient care to really get the patient to where they need to be. It's essential to acknowledge that these concerns are internal to the clinician and not the patient, and it's the clinician's responsibility to address them professionally.
The key to managing these difficulties lies in recognising that our treatment planning options are not a binary choice. It's not about exclusively embracing one extreme or the other, as often seen in social media debates. We should resist the urge to limit our choices to one end of the spectrum solely because we want to distance ourselves from the negative representations of the opposite end. In practice, elements from both ends of the spectrum can coexist within an optimal treatment plan. A comprehensive plan doesn't necessarily lead to increased patient dependency or reduced self-efficacy. Likewise, a streamlined plan doesn't imply short-changing the patient or yielding incomplete outcomes.
It's probably fair to say that most patients prefer a comprehensive care approach, especially at the start of their treatment. As they progress and gain confidence, they often lean towards more self-directed care. But, it's essential to recognise that we can sometimes misinterpret what truly matters to a patient, especially when our own biases come into play. The truth is, it's much easier to simply talk about how we can shape a treatment plan to fit different ends of the spectrum or find some happy middle ground. We can discuss the upsides and downsides of each approach and then let the patient take the lead. It’s still important that we weigh in with our professional judgment. It’s possible that some patients, when given the option, will voice a preference for a treatment pathway that is not in their best interest. In these cases, its important that our own biases don't influence our judgment about what genuinely serves the patient's well-being.
It's all quite a challenge, right? But how awesome is it that we get to do this for a living? As we keep working on understanding how our colleagues think and make clinical decisions, we might just find that embracing ideas from the end of the spectrum we've been unsure about isn't as bad for us or our patients as we once thought. Here's to our shared dedication to patient-centered care!